News Alert: New ePCR Integration Simplifies EMS Data Management and Enables Better Care Coordination
7 Essential Elements for a High-quality Patient Care Report
More so today than in the past, the need for healthcare professionals to write and maintain accurate, high-quality and detailed documentation has been a focus for institutions and providers across the healthcare spectrum including EMS services
Was this information valuable?
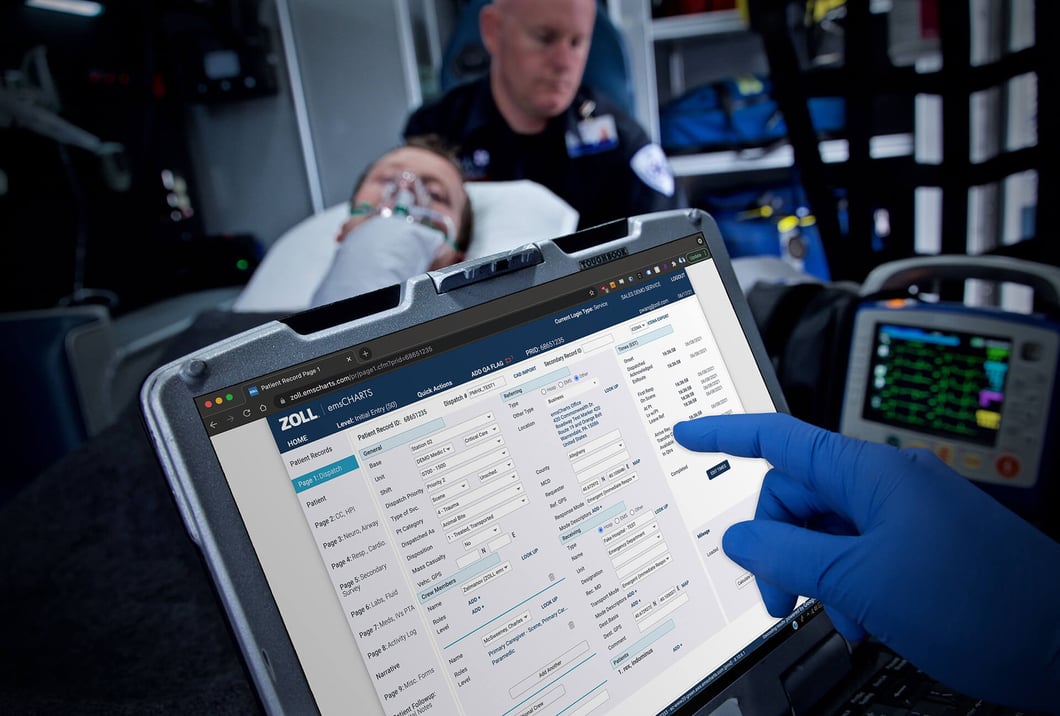
More so today than in the past, the need for healthcare professionals to write and maintain accurate, high-quality and detailed documentation has been a focus for institutions and providers across the healthcare spectrum including EMS services. As healthcare professionals (yes, EMS providers are indeed healthcare professionals), we have a responsibility to ensure that our documentation of our interaction with a patient is documented appropriately. Electronic patient care reporting (ePCR) sofware, such as ZOLL® emsCharts® and its mobile companion app, ZOLL emsCharts NOW, has given EMS professionals another tool to help us with documentation. Although there are some distinct benefits to using an electronic patient care reporting system, we must keep in mind that this is just one tool in our toolbox.
How To Write a Complete Patient Narrative
 With any system, we must keep in mind that “Garbage In = Garbage Out.” ePCR software will only produce great documentation if the data that is put into the system is accurate, thorough, and of sufficient quality. One area of documentation where providers have a significant amount of input is the narrative. One of the biggest benefits with electronic systems is the unlimited space they give providers to write their narrative. Some “seasoned” providers recall how difficult it was to cram the entire narrative into 10 or 20 lines on paper forms. Even for those select few that had the unique ability to write neatly, it proved to be a challenge. Providers now can now write a narrative without confining it into a few lines. The biggest questions now are, "What to write in my narrative? What should be included? What should I not include?"
With any system, we must keep in mind that “Garbage In = Garbage Out.” ePCR software will only produce great documentation if the data that is put into the system is accurate, thorough, and of sufficient quality. One area of documentation where providers have a significant amount of input is the narrative. One of the biggest benefits with electronic systems is the unlimited space they give providers to write their narrative. Some “seasoned” providers recall how difficult it was to cram the entire narrative into 10 or 20 lines on paper forms. Even for those select few that had the unique ability to write neatly, it proved to be a challenge. Providers now can now write a narrative without confining it into a few lines. The biggest questions now are, "What to write in my narrative? What should be included? What should I not include?"
There are many different formats available to help and guide providers with narrative documentation. For example, pick an acronym, any acronym – SOAP, SOAPIER, CHARTE – and use it as a tool to write great patient care reports. Over the past few years, the need to include additional information that doesn’t fall neatly into one of the acronym headings has grown significantly. If you extend this beyond the typical 911 EMS call, and look at what needs to be documented on acute and non-emergent, routine transfers, writing an ePCR that meets the approval of your clinical operations, CQI/QA and Billing Departments may seem like you are putting together the final components of a doctoral dissertation.
Include These Seven Elements To Paint a Complete ePCR Picture
Whether you choose one of the standard documentation formats mentioned earlier, use a service-mandated format or use a home-grown version, understanding and documenting key elements of the call in the narrative will take documentation to the next step. The contents of a high-quality narrative are already there, in the run itself. EMS providers just need to pull the information together and write it down in a way that paints a picture. There are seven elements (at a minimum) that we have identified as essentials for documenting a well written and complete narrative.
1. Dispatch and Response Summary. The dispatch and response summary provides explicit details of where the unit was dispatched, what they were dispatched for, and on what priority. Included in this section is a short description of the response itself. Did the unit arrive without incident? Was there a change in response mode?
2. Scene Summary. The Scene Summary details what happened when the crew arrived on scene. What did the scene look like? Where was the patient found? How was the patient found? What was your initial impression of the patient?
3. HPI/Physical Exam. Here is where you would detail your initial physical exam of the patient. All patient encounters should have an initial exam. The initial exam allows for the patients baseline to be established.
4. Interventions. Under this section is where all interventions are listed. What did you do to or for the patient? Interventions may include: Vital signs assessed; oxygen via NRB at 15 lpm applied; IV initiated; what medications were administered; etc. If your PCR system allows you to detail interventions elsewhere, then you just need to provide a brief overview of them here.
5. Status Change. Was there any change in the patient’s condition? If so, what was that change and what was done about it. In some situations, where there are significant changes to the patient’s condition, you may need to re-document a physical exam, interventions and status change.
6. Safety Summary. The safety summary details a couple of different things. It details how the patient was transferred from the scene to the stretcher and then to the ambulance. It also details what safety measures were performed, such as safety straps, while transferring the patient. You should also include in this section what position the patient was transferred in any other relevant information highlighting how you kept your patient safe during the transport.
7. Disposition. Disposition details the transport from the scene to the receiving facility. Like the response summary, you want to be sure to detail what facility you transported to and what priority. Was there any entry notification or was a code team such as a Trauma Team or Code AMI Team activation requested? This section also provides details as to what happened at the receiving facility. Where was the patient left? Who was care transferred to? Was report given? To who? Where there any patient belongings left? Who took control of them?
As healthcare providers, we have a responsibility to provide high-quality, accurate and detailed summaries of all patient encounters and there are a wide variety of charting tools to help EMS providers in accomplishing this. Over the years, what EMS providers need to include in their documentation has and will continue to change. The seven essential elements are designed to be another tool to help providers and services identify key elements that need to be documented for every encounter and provides a framework for putting it to paper (or computer).
Read More About How Technology Can Help Ensure High-quality Patient Care Reports:
App Lets You Keep Charting Through the Chaos
Related Posts
How STAT MedEvac Connected Device, Software, and Data Technology To Enhance QA and Elevate Care
Podcast: 4 Ways ePCR Software Can Relieve EMS’ Biggest Headaches
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS & fire, hospital, or AR professional easier.
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS, fire, hospital, or AR professional easier.





