A Patient-Centered Learning Healthcare System: The EMS of the Future
Welcome to part three of the three-part series focusing on healthcare reform and the future of Emergency Medical Services (EMS)

Welcome to part three of the three-part series focusing on healthcare reform and the future of Emergency Medical Services (EMS). In part one, we reviewed the key concepts of healthcare reform, including the Triple Aim, patient navigation, and the ability to access a patient’s electronic health information. In part two, we focused specifically on Health Information Exchange (HIE) and four key EMS use cases where HIE directly impacts operational and patient outcomes. In this piece, we will finish up this series with a vision of the future for EMS in a patient-centered learning healthcare system.
In 2015, the Institute of Medicine (IOM) presented a concept of a “Learning Healthcare System.” This was defined as a system in which “science, informatics, incentives, and culture are aligned for continuous improvement and innovation, with best practices seamlessly embedded in the delivery process and new knowledge captured as an integral by product of the delivery experience.” Earlier in 2001, the IOM defined another concept, “Patient-Centered Care,” as “providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions.”
The future of healthcare is often described by combining these two concepts into a Patient-Centered Learning Healthcare System. To be successful, we must leverage healthcare Information Technology (IT) including electronic health records and health information exchange to improve health, health care quality, safety, and communication for all members of the care team. It is important to note that the healthcare provider (especially EMS) and the patient are considered members of the healthcare team.
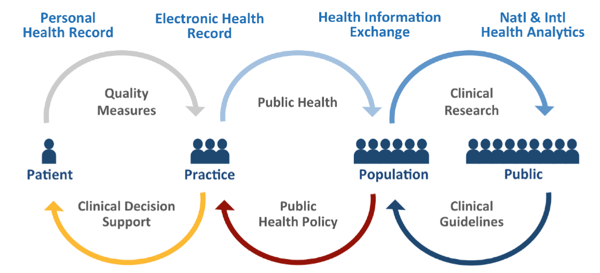
The diagram below describes the concept of a Patient-Centered Learning Healthcare System:
- Healthcare information begins with the patient’s personal health record that is integrated into an overall electronic health record that is accessible to other providers and included in health analytics.
- Quality measures drive systems of care, standardize care delivery, research, and safety.
- Research and Analytics drive clinical guidelines, health policy, and clinical decision support.
ONC Vision of the Health IT Ecosystem and Patient-Centered Care
So, how does this impact EMS and is this really… The Future of EMS?
We have outlined, in this series, the foundational infrastructure that will enable ongoing quality measurement and clinical decision support (CDS). CDS, when effectively applied, contributes to increased quality of care, improved outcomes, error reduction (and avoidance), improved efficiency, reduced costs, and enhanced provider and patient satisfaction. CDS does not replace clinical judgement but it does provide information, guidance, insight, and a level of intelligence for making timely, informed, and higher quality decisions.
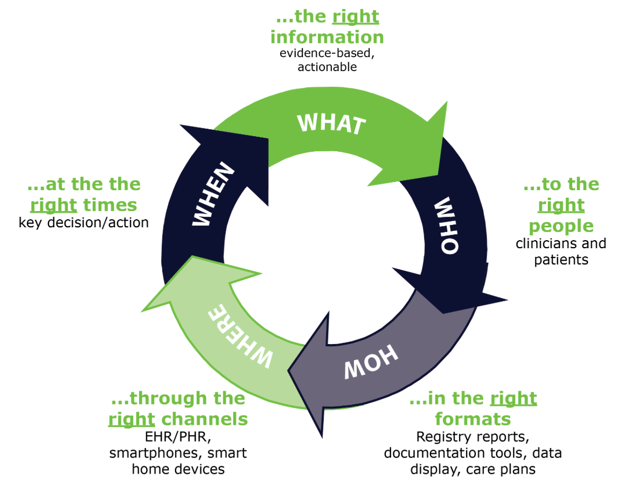
A framework for CDS known as the “Five Rights” is helpful to understand the potential of CDS.
In summary, data, along with the devices that collect and analyze it, were once tools in our tool belt used as needed in the provision of patient care. Through CDS, data and devices become much more than that... they are a member of our healthcare team. This is the future of EMS.
Related Posts
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS & fire, hospital, or AR professional easier.
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS, fire, hospital, or AR professional easier.




