News Alert: New ePCR Integration Simplifies EMS Data Management and Enables Better Care Coordination
Advancing the Continuum of Care
The Time to Become Step 1 in Your Community’s Continuum of Care is Now Too often in our pursuit of a “smart system” on which to base our EMS decisions, we find ourselves bound and limited by the very technology we implement to overcome process obstacles
Was this information valuable?

The Time to Become Step 1 in Your Community’s Continuum of Care is Now
Too often in our pursuit of a “smart system” on which to base our EMS decisions, we find ourselves bound and limited by the very technology we implement to overcome process obstacles. Although we put a system in place that effectively solves one problem, we sometimes learn days or weeks later that we simultaneously made another process harder, or added extra steps to an otherwise simple interface. For these reasons, it has been extremely important to us at JFK EMS that our ePCR program is not only adaptable and customizable, but also able to keep up with the pace of innovation and change we maintain as a progressive EMS system. I can think of no more obvious example of this when it comes to RescueNet ePCR than in the case of our sepsis protocol.
 JFK EMS is a hospital-based EMS system in Edison, New Jersey, providing basic and advanced life support services to the state’s fifth most populous municipality and the surrounding towns across three counties. EMS is special in New Jersey, with ALS and BLS responses organized into a two-tiered system, and all ALS required to be hospital based. This creates a mixed bag of response possibilities at the BLS level, from volunteer to fire-based to municipal to hospital-based like us; and sets our EMS organization up to be the logical liaison to all of these entities for our hospital system. As hospital metrics and reporting necessities extend further and further into the field – prior to patients actually entering the doors of the hospital – we find our health system increasingly aware of the role of all levels of EMS in the continuum of care, and increasingly interested in making sure these relationships exist at a functional level. As I’m sure many of you know, this is a challenge, and often feels like a full-time job in and of itself.
JFK EMS is a hospital-based EMS system in Edison, New Jersey, providing basic and advanced life support services to the state’s fifth most populous municipality and the surrounding towns across three counties. EMS is special in New Jersey, with ALS and BLS responses organized into a two-tiered system, and all ALS required to be hospital based. This creates a mixed bag of response possibilities at the BLS level, from volunteer to fire-based to municipal to hospital-based like us; and sets our EMS organization up to be the logical liaison to all of these entities for our hospital system. As hospital metrics and reporting necessities extend further and further into the field – prior to patients actually entering the doors of the hospital – we find our health system increasingly aware of the role of all levels of EMS in the continuum of care, and increasingly interested in making sure these relationships exist at a functional level. As I’m sure many of you know, this is a challenge, and often feels like a full-time job in and of itself.
Advancing the Continuum of Care
But for those of us who remember a time when many hospitals seemed ambivalent (at best) toward the existence of their “ambulance drivers,” and the necessary relationship they were forced to maintain with us through the Certificate of Need system in New Jersey, this rediscovered interest has been exactly the in road we have been waiting for. By requiring more quality-related data from the step in the process that happens prior to hospital arrival, CMS and other regulatory data collection agencies have provided a ready-made conduit for legitimizing who we are and what we do in EMS. Sure it seems like a lot of extra work in many cases, and we may find ourselves prioritizing clinical and operational initiatives differently based on the external stakeholders we are attempting to impress. If, however, the end result is more resources for EMS from partners in healthcare allowing for more complete and correct patient care, isn’t this a win-win?
In many instances, the blueprint is already laid out for us. When we encounter a patient with chest pain, the standard of care isn’t only to treat with aspirin, nitro, etc. clinically. The standard is also to transmit a 12-Lead to the receiving facility and initiate a pre-hospital alert to ensure that the next steps in the continuum are as prepared, ready and waiting as possible. National standards for door-to-balloon reinforce EMS’ part in this practice, and expanded reporting through the ACTION registry now entrenches the EMS PCR as necessary documentation with first medical contact-to-balloon becoming a necessary field in this reporting process.
As is usually the case, stroke care is not far behind, with intensifying research calling much-needed attention to CVA destination protocols. In this case, however, the path forward isn’t finalized. The American Heart Association/American Stroke Association has proposed an algorithm based on using severity scoring systems to attempt to predict large vessel occlusion. But before some states are willing to create policy that will divert patients from primary stroke center stakeholders, they are asking valid sensitivity and specificity questions about the assessments being employed. This is clearly a case where a robust, customizable EMS ePCR system like ZOLL’s can be configured to collect, analyze and share data that should be used to craft the way forward on this extremely important issue.
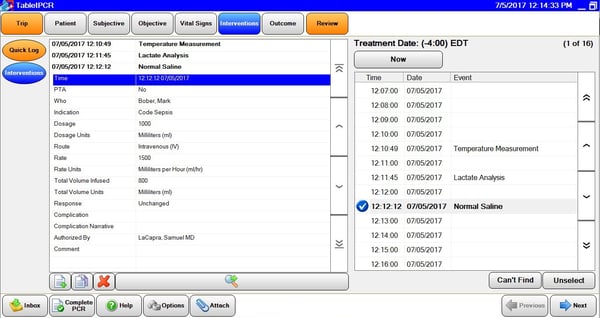
The Role of Data Integration to Improve Compliance & Performance
Here at JFK EMS, we also saw opportunity to provide value for our health system in the pre-hospital sepsis arena. When we tackled the sepsis issue, we did so from the perspective of what would be in the patient’s clinical best interest and with the idea that we could help the hospital improve compliance and performance. In many ways, being hospital-based in New Jersey allows for partnerships, data access and process integration that are hard to come by in other parts of the country. Such is the case with sepsis, and the combination of presence on the steering committee and seamless data integration through our HL7 import has proven to be the one-two punch we needed. Through close collaboration with the hospital’s Quality Assurance and Regulatory Compliance personnel, we were able to sculpt the temperature measurement, lactate level analysis, lab draw, fluid administration and blood pressure support interventions so that they directly mirror the information contained in the ED charting systems and meet all necessary CMS reporting requirements. Guidance and decision support documents were also placed in ePCR in the help menu for easy access, ensuring that our providers perform the right interventions and chart them the right way to meet all stringent reporting requirements. This provides the emergency department with an early recognition and treatment resource as well as a reliable reporting structure capable of dotting necessary regulatory I’s and crossing compliance T’s.
Sure it requires more work on our part, both for our front line providers with our patients in the field and for quality assurance and data collection personnel within the EMS department. But we believe this additional effort is well worth it for two primary reasons:
- First, sepsis patients are being identified earlier, treated earlier and vigilantly assessed from the time of ED arrival to the time they are transferred to a floor, improving morbidity and mortality as well as shortening length of stay for these people. We all signed on in this field to help people above all else, and if we can make our health system look better while doing exactly that, what’s not to like?
- And second, when you make your partner health system look better, they look for ways to help you keep doing it. In this particular case, funding for our thermometers and lactate meters was heavily subsidized by the organization.
Breaking Down Silos Between EMS & Hospitals
It’s a turbulent time in American health care. Being able to predict the future of reimbursement and how it affects our bottom line in EMS probably requires more than a crystal ball and a flux capacitor at this point. But if one thing above all others seems certain, doing more with less is most likely going to be our reality for years to come. With the “silver tsunami” about to come crashing down on our heads, the goal has to be maximizing the doing more and minimizing the less with which we do it. Often that involves adapting, breaking traditional molds of inward thinking and evaluating ways to plug in and assist our partner stakeholders in health care. Thinking like an EMS agency relegated to the silo of pre-hospital care will not be enough to sustain our mission moving forward. The time to become the essential Step One in your community’s continuum of care is now, and proving the various creative and novel ways we can add value to that continuum should be our primary focus across our profession as we attempt to prepare for whatever comes next.
Related Posts
How STAT MedEvac Connected Device, Software, and Data Technology To Enhance QA and Elevate Care
Podcast: 4 Ways ePCR Software Can Relieve EMS’ Biggest Headaches
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS & fire, hospital, or AR professional easier.
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS, fire, hospital, or AR professional easier.