4 Must-have Data Points for Dispatch-Billing Alignment and Maximum Reimbursement
Demystifying Proper EMS Billing for Hospital Inpatient Transports Part 2: Medicare Bundling Rules
This post is Part Two of a three-part series
Was this information valuable?

This post is Part Two of a three-part series. View Part One | View Part Three.
In the previous installment of this three-part article series, we examined the different types of payers and how the billing rules are significantly different if the patient is covered by Medicare, Medicaid, a commercial insurer, or is a self-pay. Now let’s turn our attention to the sometimes-complicated Medicare bundling rules that apply to hospital inpatients.
In the previous installment of this three-part article series, we examined the different types of payers and how the billing rules are significantly different if the patient is covered by Medicare, Medicaid, a commercial insurer, or is a self-pay. Now let’s turn our attention to the sometimes-complicated Medicare bundling rules that apply to hospital inpatients.
Medicare Bundling Rules
If you transport a hospital inpatient who is covered by Medicare, there are several questions you’ll have to answer to determine who to bill.
Before we delve into the specific rules, let’s take a quick look at the basic Medicare bundling concept. Medicare shifted much of its payment strategy over the years to put more financial responsibility on hospitals and other facilities. Part of that strategy was to “bundle” the billing for Medicare patients who are admitted to a hospital. This means that Medicare pays the hospital a set amount of reimbursement, under Part A, that is determined prospectively by the patient’s admitting diagnosis. With some exceptions, any outside healthcare service providers must generally bill the facility for their services instead of separately submitting a bill to the Medicare program for payment under Part B. In hospitals, this prospective, bundled reimbursement amount paid to hospitals is based on Diagnosis Related Groups (DRG), a system which was implemented in the 1980s. Remember that DRG-based inpatient bundling applies to Medicare, because the law says so. It does not automatically apply to non-Medicare payers, and it is imperative to identify the proper primary payer first.
Now, let’s get into some of the specifics.
Origins and Destinations. Medicare inpatient ambulance transports require you to first determine whether the patient is being transported to another location and then returned to the hospital of origin (i.e., “non-discharge transports”), or whether the patient is being transported to another facility altogether (i.e., “interfacility transports).”
First, let’s dispense with an easy one: a patient being transported to a hospital emergency department from a scene of an emergency (e.g., home or an accident scene) is not subject to the Medicare inpatient bundling rules, even if the patient is subsequently admitted as an inpatient. This transport is covered by Medicare provided that the normal coverage rules, such as medical necessity and nearest appropriate facility, are met. By the way, if those coverage criteria are not met, then the transport is billable to the patient as a non-covered service, and your agency may charge its full retail rate and apply any hardship criteria it may have in place.
Next, if a Medicare hospital inpatient is being transported to another location for a service that is not available at the origin hospital, and returned to the hospital of origin, the patient does not lose their inpatient status at the hospital of origin. Therefore, such a transport is billable to the hospital in almost all cases. In fact, Medicare’s claim processing system has “edits” (i.e., filters) in place to automatically deny Part B claims for transports occurring between the admission and discharge dates for hospital inpatients.1
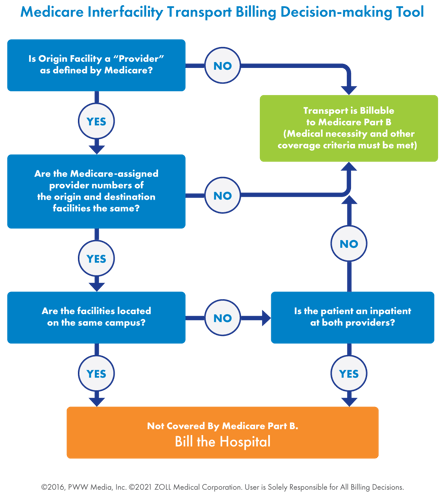
Now, let’s look at Medicare hospital inpatients who are transported from a hospital to another facility and not returning to the hospital of origin. There is a specific set of rules, which we call the Medicare “three-part test,” for determining who to bill for this interfacility transport.2
The Three-part Test
Part One. The first criteria when transporting a Medicare inpatient from a hospital to another facility is to look at the Medicare provider numbers of the origin facility and the destination facility. Please note that we are referring to the Medicare-assigned provider number, not the facility’s National Provider Identifier (NPI) number. This Medicare provider number is sometimes called a Provider Transaction Access Number (PTAN).
If the Medicare provider numbers of the two facilities are different, the transport is billable to Medicare Part B, provided that all applicable coverage criteria (e.g., medical necessity, nearest appropriate facility, etc.) are satisfied.
If the Medicare provider numbers of the two facilities are the same, it is necessary to go to Part 2 of the three-part test.
Part Two. If the Medicare provider numbers of the origin and destination facilities are the same, the next thing to look at is whether they are on the same campus or different campus. Most interfacility transports will be between facilities on different campuses. If the facilities are on the same physical campus, as defined by Medicare, the transport must be billed to the hospital and cannot be billed to Medicare. If the facilities are on different campuses (which is usually the case) you then proceed to Part 3.
Part Three. If the Medicare provider numbers of the two facilities are different, and the interfacility transport is between facilities on different campuses, you must determine whether the patient was an inpatient at both the facility of origin and the destination. If you pick up a Medicare hospital inpatient and transport them to a facility with the same Medicare provider number on a different campus, and the patient is directly admitted as an inpatient at the second facility, the transport is properly billed to the hospital.
If the patient is not an inpatient at both the origin and destination facilities, the transport is billable to Medicare Part B, provided that all coverage criteria are met.
Some Notes on the Three-part Test
There are a few quirks to look out for when it comes to properly applying the three-part test for Medicare hospital inpatients transported to another facility. First, when determining whether the patient is an inpatient at both facilities, be aware that inpatient status is defined by Medicare rules. It is not necessarily the same thing as being in an inpatient bed. For Medicare purposes, an admission occurs when an admitting physician writes an order for admission. In that case, admission may begin even before a patient lands in an inpatient bed.
Here’s an example. Say, for instance, that a physician determines that a Medicare patient in the emergency department at Hospital A requires admission, but the only beds available are at Hospital B, which is the hospital’s sister facility. The two facilities share a Medicare provider number and are on different campuses. The emergency department (ED) physician at Hospital A has admitting privileges at Hospital B and writes the admission order for the patient in the ED prior to transport. Under Medicare rules, the patient becomes an inpatient when the physician writes the admission order. So, when the ambulance picks up the patient at Hospital A’s ED, they are an inpatient – even though the ED is an outpatient department. If the patient is then transported to Hospital B and admitted, the transport must be billed to the hospital, not to Medicare.
Another wrinkle in the three-part test is that even a freestanding ED (FSED) can be considered a hospital if it has elected “provider-based status” for the FSED.3 If the FSED is provider-based, you’ll need to apply the three-part test as if the FSED was a hospital. If the FSED is not provider-based, then the transport would not be covered by the three-part test, and you would bill Medicare for the transport from the FSED to the destination hospital, provided of course that the transport meets all the usual coverage criteria (medical necessity, nearest appropriate facility, etc.)
One final wrinkle: even if an admitting physician writes an admission order for a patient, and the patient is transported from Hospital A to Hospital B, the patient must then actually be admitted at Hospital B for the three-part test to apply. Say, for instance that the ED physician at Hospital A writes the admission order and the ambulance transports to Hospital B for admission, but it is later determined at Hospital B that the patient does not require admission after all, and they are sent home. Because the patient never ended up being admitted at Hospital B, the transport is not billed to the hospital; it is billable to Medicare if all of the applicable coverage criteria are met.
Next time, in Part Three of this article series, we’ll answer the question, “How much of the bill must the hospital pay?” Stay tuned.
Read More:
Demystifying Proper EMS Billing for Hospital Inpatient Transports Part 1: Who’s the Payer?
1 Medicare Claims Processing Manual, Chapter 3 – Inpatient Hospital Billing, Sections 10.4 and 10.5.
2 Medicare Claims Processing Manual, Chapter 10 – Ambulance Services, Section 10.3.3.
3 42 C.F.R. § 413.65.
Related Posts
How Right-day Billing With Automated Deductible Monitoring Can Increase Provider Revenue
Maximize Revenue and Reduce Bad Debt by Monitoring Deductible Status
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS & fire, hospital, or AR professional easier.
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS, fire, hospital, or AR professional easier.




