Chart Smarter: Why One EMS Agency Ditched Paper for Mobile Tech
Not Your Traditional EMS Call: Documentation and Billing for Telehealth Consults
(5 min read)
Was this information valuable?

(5 min read)
Gaps in Pre-populated ePCR Options Mean New Processes for Documenting Billable Activities
Telehealth, telemedicine, or whatever tele-variation it goes by, is gaining popularity in the prehospital care industry, thanks especially to COVID-19. What was once thought of by EMS providers primarily as a tool in the mobile integrated healthcare/community paramedicine (MIH/CP) arena, is now being examined as an early 911 call screening tool. This raises a valid question: how should we document telehealth utilization? After all, telehealth consults aren’t the same as our traditional EMS call.

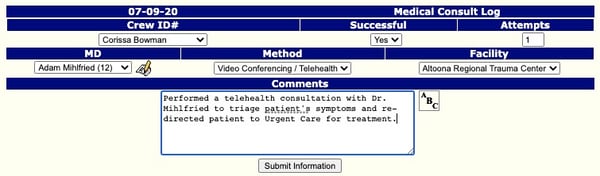
Defining a Call Versus an Encounter
It all starts with the reason a telehealth consult is being utilized. If you’re incorporating a telehealth consult into your early assessment process to screen for COVID-19 symptoms, verify your stroke assessment findings with an on-call neurologist, or even to walk through a complicated case with an online medical control physician, then you’re utilizing telehealth in the context of a “call.” This likely requires documentation of the event in your electronic patient care report (ePCR) software. The current issue with many platforms, however, is that there probably is not a drop-down option for “telehealth consult” in your flow chart or assessment tabs. Therefore, you’ll need to address your documentation procedure if your agency is looking to implement telehealth services. You will need to document a medical consult, specifying clearly that it was for telehealth. Best-in-class ePCR software will enable you to build custom assessments to capture other details, as seen in the example below, for telehealth:
Then there are the events classified as “encounters,” which do not result from an emergency call. Instead, they’re more typical of the telehealth visits included in an MIH/CP program. While medics might still be assessing a patient, they’re not doing so in the traditional “call” sense, where there’s a turnout time or even a formal “response.” In these situations, it wouldn’t be appropriate to document your entire patient encounter under a “treatment, without transport” disposition because the preliminary portion of this event wasn’t initiated with a “call” requesting a “response.”
Documenting encounters incorrectly as calls will only invalidate your data for tracking purposes, as you haven’t selected the best option. While there may be a billing opportunity here, that doesn’t make it an appropriate use of your standard ePCR platform’s capabilities. Functioning MIH/CP programs truly require a documentation functionality unique to this type of program, especially where telehealth consults are concerned.
Examples of MIH/CP Telehealth Documentation Practices
- Referencing patient care encounters over time, rather than an isolated instance
- Setting up care plans and progress reports
- Providing single (per encounter) assessments, while not having to abide by traditional EMS PCR completion rules
- Signature rules that differ from EMS PCR, with an opportunity to create standing approvals for assessment and HIPAA privacy
- Avoiding tracking encounters as “Treatment, No Transport” incidents (which are 911-oriented)
Direct Versus Indirect Documentation
During the course of a traditional EMS call, you’re documenting from the first-person point of view. During a telehealth consult, the point of view may change to third person, such as when you are capturing the details of a conversation between yourself and the online physician, specialist, or other care provider with whom you’re consulting. Here’s a typical example to illustrate the difference:
“We splinted the patient’s arm with padded board splints and cravats in a position of comfort, which CMS assessed as positive in all four extremities before and after the intervention.”
Versus:
“The consulting physician advised that she recommended a change in the patient’s furosemide dosage to reflect an acute exacerbation of the patient’s CHF and pulmonary edema symptoms.”
Where to document all of this, of course, will be dependent upon the set-up of your ePCR platform. Is there a “telehealth consult” option under your assessment tab, or does it fall under intervention options in your flow chart? Your documentation approach could significantly improve or hamper your billing opportunities. This issue will only continue to gain prominence as telehealth gains momentum as a revenue stream for the EMS industry. It’s wise to do your homework and formalize your documentation process now so that all your crews know the right way (and the wrong way) to capture telehealth services.
One factor that has yet to be addressed is whether or not EMS or MIH/CP providers can bill while acting as a middleman. Again, directly versus indirectly, when EMS agencies respond to a call or perform a procedure, they bill for it because they provided the care. If, on the other hand, EMS simply acts as the middleman between a patient and another provider, can they bill for the service of being a proxy? Does this present a double-invoice situation? Telemedicine can muddy the water a little bit, so taking the extra steps to carefully document your actions — both directly and indirect — could make or break your case for billing for your services.
Much More to Learn
With telehealth, we’re certainly writing a new chapter in the life of EMS, which means that we have much more to learn regarding the finance, logistics, operations, and planning related to this new mode of care. It’s an exciting time, quite honestly! We have the ability to shape how prehospital healthcare and paramedicine looks, and we can even influence health information exchange (HIE) as we push to integrate documentation standards spanning PCR/EMR and MIH/CP platforms and providers. Telehealth is just the beginning of the potential range of services EMS may provide in the near future, and it’s definitely an innovative leap in the way we “respond” to our traditional “call.” We just need to remember that with innovative services come new implications for billing. At the end of the day, we need to make sure that we document appropriately so that we can capture maximum revenue for the work we do.
Read about the best practices for capturing telehealth revenue:
Innovating Revenue Streams During COVID-19: Four Best Practices
Related Posts
The End of Delayed Documentation
News Alert: New ePCR Integration Simplifies EMS Data Management and Enables Better Care Coordination
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS & fire, hospital, or AR professional easier.
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS, fire, hospital, or AR professional easier.




