News Alert: New ePCR Integration Simplifies EMS Data Management and Enables Better Care Coordination
Taking a Deeper Look at the Guidelines for CPR
Not so long ago, professional rescuers were taught the same things as civilians when it comes to CPR — push hard, push fast
Was this information valuable?

Not so long ago, professional rescuers were taught the same things as civilians when it comes to CPR — push hard, push fast. That was all you needed to ensure you were doing good chest compressions. The new American Heart Association (AHA) Guidelines have raised the bar. Now, there is greater specificity on the rate and depth of compressions; and we need to meet these targets if we want more patients to survive and ultimately be discharged from the hospital.
Here's a look at the AHA's key recommendations for CPR from 2015:
Chest Compression Depth. Formerly, the AHA recommended a depth of greater than 2 inches. It now says depth should fall within the range of 2 to 2.4 inches (5 to 6 cm).
Chest Compression Rate. The AHA changed its recommendation of more than 100 compressions/min to 100 to 120 compressions/min.
Chest Compression Fraction. A hot topic in the resuscitation world, this refers to the percentage of time in a code in which chest compressions are being done. The AHA's 2013 CPR Consensus Statement called for a compression fraction of at least 80 percent; the 2015 Guidelines lowered that figure to at least 60 percent. It's critical to note that in a hospital setting, the consensus is that compression fraction should be at least 80 percent.
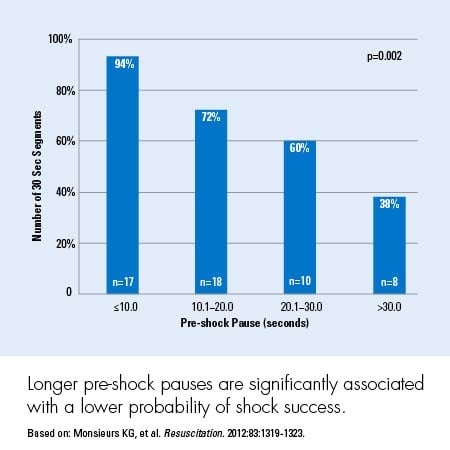
Interruptions. Every interruption during CPR is important, so we must strive to minimize those interruptions. The AHA now recommends no more than a 10-second interruption during CPR for pulse checks and pre- and post-shock pauses.
Ventilation Rate. The 2015 Guidelines recommend one breath every six seconds in intubated patients.
Chest Compression Release. The AHA now emphasizes the importance of fully releasing (allowing for full recoil) and doing so quickly.
Chest Compression Release Velocity. It's not just coming off the chest completely that is critical, but also how quickly you allow the chest to recoil. Data suggest that faster release velocity correlates with an improved survival to discharge and good neurologic status.
Capnography (end tidal carbon dioxide, or EtCO2). Given a Class I recommendation, continuous waveform capnography remains the gold standard for verifying ET tube placement and it is also becoming more popular in monitoring resuscitation progress.
Debriefing. The AHA placed a major emphasis on debriefing of both mock codes and actual resuscitations.
Feedback. The AHA gave a Class IIA recommendation to the use of devices that provide feedback on the quality of chest compressions in real time during training and resuscitation events.
When you take into account all of these recommendations, it's clear that performing chest compressions is a true skill that's difficult to master. Accordingly, it's not something that should be assigned to a provider who lacks the proper training and experience.
LEARN MORE ABOUT THE CLINICAL STUDIES INFLUENCING THE SCIENCE OF CPR
Related Posts
How STAT MedEvac Connected Device, Software, and Data Technology To Enhance QA and Elevate Care
Podcast: 4 Ways ePCR Software Can Relieve EMS’ Biggest Headaches
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS & fire, hospital, or AR professional easier.
ZOLL Pulse Blog
Subscribe to our blog and receive quality content that makes your job as an EMS, fire, hospital, or AR professional easier.